Key Takeaways
- Up to 60 percent of individuals with bipolar disorder will develop a substance use disorder during their lifetime, the highest rate of any mood disorder.
- Both manic and depressive episodes drive substance use through different mechanisms, making bipolar disorder uniquely challenging to treat alongside addiction.
- Mood stabilizers like lithium and valproate are the cornerstone of bipolar treatment and must be maintained throughout addiction recovery.
- Integrated treatment programs that coordinate psychiatric medication management with addiction counseling produce the best outcomes for this population.
Why Bipolar Disorder and Substance Abuse Co-Occur
Bipolar disorder and substance abuse form one of the most challenging co-occurring combinations in behavioral health. Research published in the American Journal of Psychiatry indicates that up to 60 percent of individuals with bipolar I disorder will develop a substance use disorder at some point in their lives. This rate is dramatically higher than the general population and represents the highest co-occurrence rate of any mood disorder.
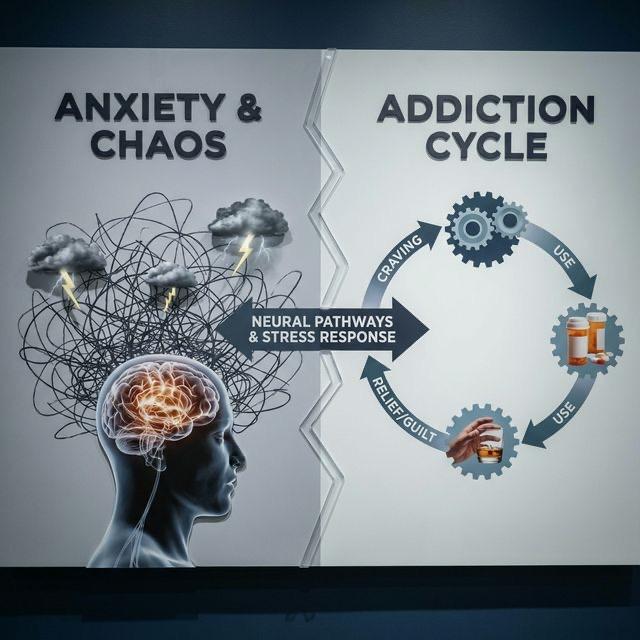
The extreme mood states that characterize bipolar disorder create distinct pathways to substance use. During manic episodes, impulsivity and sensation-seeking drive experimentation and binge use. During depressive episodes, the desire to escape emotional pain motivates self-medication. This dual vulnerability makes individuals with bipolar disorder exceptionally susceptible to addiction.
Trust SoCal in Southern California provides specialized treatment for co-occurring bipolar disorder and addiction, recognizing that standard addiction treatment approaches are insufficient for this population without concurrent psychiatric stabilization.
Bipolar disorder affects approximately 2.8 percent of the U.S. adult population, but accounts for a disproportionately large share of dual diagnosis cases due to its extremely high co-occurrence with substance use disorders.
Substance Use During Manic Episodes
Manic episodes are characterized by elevated mood, grandiosity, decreased need for sleep, racing thoughts, pressured speech, and increased goal-directed activity. During mania, judgment and impulse control are severely impaired, leading to risk-taking behaviors including substance use that the individual would typically avoid.
Stimulants like cocaine and methamphetamine are frequently used during manic episodes because they amplify the euphoric, energized feelings that mania produces. Alcohol is also commonly consumed in large quantities as part of the social excess and disinhibition that accompany manic states.
The combination of mania and substance intoxication can produce extremely dangerous behavior, including driving under the influence, financial recklessness, sexual impulsivity, and aggression. These consequences often serve as the catalyst for individuals with bipolar disorder to finally seek treatment.
Substance Use During Depressive Episodes
The depressive phase of bipolar disorder can be even more devastating than the manic phase, and it often lasts significantly longer. Bipolar depression shares many features with major depressive disorder, including profound sadness, loss of interest, fatigue, hopelessness, and suicidal ideation. These symptoms drive substance use as a means of self-medication.
Alcohol, opioids, and cannabis are the substances most commonly misused during bipolar depressive episodes. Each provides temporary emotional numbing or mood elevation that offers brief respite from the crushing weight of depression. However, each also worsens the underlying mood instability, creating a more volatile and unpredictable illness course.
The Impact on Cycling
Substance use accelerates mood cycling in bipolar disorder, increasing both the frequency and severity of episodes. Stimulants can trigger manic episodes in vulnerable individuals, while alcohol and depressants can precipitate or deepen depressive episodes. This substance-induced cycling makes the disorder progressively harder to manage.
Even cannabis, which many individuals with bipolar disorder use in an attempt to stabilize their mood, has been shown to increase the frequency of manic episodes and reduce medication adherence. The destabilizing effects of substances on bipolar cycling underscore the importance of achieving sobriety as part of mood management.
Medication Non-Adherence
One of the most significant challenges in treating co-occurring bipolar disorder and addiction is medication non-adherence. Individuals in manic states may feel so good that they believe they no longer need medication. During depressive episodes, hopelessness may lead them to abandon their treatment regimen. Substance use further compromises adherence by impairing memory, judgment, and routine.
This non-adherence creates a dangerous cycle: stopping mood stabilizers leads to more severe episodes, which drive more substance use, which further disrupts medication compliance. Breaking this cycle requires structured support and monitoring throughout the treatment and aftercare process.
Diagnostic Challenges
Diagnosing bipolar disorder in the context of active substance use is exceptionally difficult because substance intoxication and withdrawal can mimic both manic and depressive episodes. Cocaine-induced euphoria resembles mania, while alcohol withdrawal can produce agitation and insomnia that mimic hypomanic states. Post-stimulant crashes closely resemble depressive episodes.
Accurate diagnosis often requires a period of monitored sobriety during which clinicians can observe the client's natural mood patterns. Family history of bipolar disorder, the presence of symptoms before the onset of substance use, and the persistence of mood symptoms during sustained sobriety all provide important diagnostic clues.
Trust SoCal's clinical team includes psychiatrists experienced in differentiating bipolar disorder from substance-induced mood disturbances. Our structured intake process allows for the extended observation and comprehensive assessment that accurate diagnosis requires.
Integrated Treatment for Bipolar Disorder and Addiction
Effective treatment for co-occurring bipolar disorder and substance abuse requires simultaneous attention to both conditions through a coordinated clinical team. Treating addiction without stabilizing mood leads to relapse driven by untreated episodes. Treating bipolar disorder without addressing addiction leaves the most common destabilizing factor in place.
Pharmacological Management
Mood stabilizers, particularly lithium and valproate, form the pharmacological foundation of bipolar treatment and must be maintained throughout addiction recovery. Atypical antipsychotics such as quetiapine and aripiprazole may also be used, with quetiapine showing particular promise for reducing both mood symptoms and alcohol consumption in dual diagnosis populations.
Medication-assisted treatment for addiction, including naltrexone for alcohol use disorder, can be safely combined with most mood stabilizers. Our medical team at Trust SoCal creates comprehensive medication plans that address both conditions without harmful interactions.
Psychoeducation and Self-Management
Psychoeducation about bipolar disorder is a critical treatment component that helps clients understand their illness, recognize early warning signs of mood episodes, and develop proactive management strategies. When clients understand how substance use destabilizes their mood cycling, they gain powerful motivation for maintaining sobriety.
Self-management skills include mood charting, sleep hygiene practices, stress management techniques, and the development of a personal crisis plan that outlines steps to take when mood symptoms intensify. These tools empower clients to take active roles in managing their condition long after formal treatment ends.
The Critical Role of Sleep in Bipolar Recovery
Sleep disruption is both a symptom and a trigger of bipolar episodes, and it is profoundly worsened by substance use. Even a single night of significantly reduced sleep can trigger a manic episode in vulnerable individuals. Alcohol, stimulants, and cannabis all disrupt normal sleep architecture in ways that destabilize mood.
Establishing healthy sleep habits is therefore a cornerstone of dual diagnosis treatment for bipolar disorder. This includes maintaining consistent sleep and wake times, avoiding caffeine after noon, creating a cool and dark sleep environment, and developing a calming pre-sleep routine. Melatonin and certain non-addictive medications may also be used to support sleep regulation.
At Trust SoCal, our treatment schedule is designed to support regular sleep patterns, and our clinical team monitors sleep quality as an important indicator of mood stability throughout the treatment process.
Never discontinue mood stabilizers or other bipolar medications without medical supervision, even if you feel stable. Abrupt discontinuation significantly increases the risk of a severe mood episode and can be dangerous.
Long-Term Recovery and Relapse Prevention
Recovery from co-occurring bipolar disorder and addiction is a lifelong process that requires ongoing psychiatric care, addiction support, and vigilant self-management. Relapse prevention planning for this population must address both conditions, with specific strategies for managing mood triggers and substance triggers.
A comprehensive aftercare plan should include regular psychiatric appointments for medication monitoring, continued therapy, participation in support groups, maintenance of healthy lifestyle habits, and a clear action plan for what to do if mood symptoms or cravings intensify. With proper support and commitment to treatment, individuals with bipolar disorder and addiction can achieve stable, fulfilling lives in recovery.

Rachel Handa, Clinical Director
Clinical Director & Therapist